I'm not feeling good . We had a brief discussion with professor regarding pathogenesis of anthrax, the toxin production, ect ect ect. It was pretty good at first because we are discussing but it turned us down because he asked about BLOOD CLOTTING MECHANISM. Oh my god, I hardly remember any of them :( It made me realised that there are many things i have left out. Oh my,,
*********************************************************
How does the bleeding is stopped?
Blood coagulation refers to the process of forming a clot to stop bleeding. There are 3 mechanisms that work together to stop the flow of blood. They are;
1. Vasoconstriction
2. Platelet plug formation
3. Clotting of blood
Vasoconstriction of a damaged blood vessel slows the flow of blood and thus helps to limit blood loss. This process is mediated by:
Local controls. Vasoconstrictors such as thromboxane are released at the site of the injury.
Systemic control. Epinephrine released by the adrenal glands stimulates general vasoconstriction
Systemic control. Epinephrine released by the adrenal glands stimulates general vasoconstriction
Platelet plug. Platelets aggregate to the site of the injury. They stick together acting as a "plug." Platelets also activate the process which causes a fibrin clot to form, known as secondary hemostasis. Platelets stick to collagen and become activated. Activated platelets release chemicals such as ADP, and thromboxane, that cause the aggregation of more platelets to the site of injury. Platelet aggregation results in the formation of a platelet plug which acts to stem the flow of blood from the broken vessel. It is essential that platelets become activated only at the site of a broken vessel. Otherwise activated platelets would form plugs and induce clots in inapropriate places. Healthy vessels secrete an enzyme called prostacyclin that functions to inhibit platelet activation and aggregation.

Secondary hemostasis
Platelets alone are not enough to secure the damage in the vessel wall. A clot must form at the site of injury. The formation of a clot depends upon several substances called clotting factors. These factors are designated by roman numerals I through XIII. These factors activate each other in what as known as the clotting cascade. The end result of this cascade is that fibrinogen, a soluble plasma protein, is cleaved into fibrin, a nonsoluble plasma protein. The fibrin proteins stick together forming a clot.
The blood contains about a dozen clotting factors. These factors are proteins that exist in the blood in an inactive state, but can be called into action when tissues or blood vessels are damaged. The activation of clotting factors occurs in a sequential manner. The first factor in the sequence activates the second factor, which activates the third factor and so on. This series of reactions is called the clotting cascade.
Blood clotting is the transformation of liquid blood into a semisolid gel. Clots are made from fibers (polymers) of a protein called fibrin. Fibrin monomers come from an inactive precursor called fibrinogen. The body of the fibrinogen molecule has caps on its ends that mask fibrin-to-fibrin binding sites. If the caps are removed then fibrin monomers polymerize to form fibrin polymers. This process requires thrombin, the enzyme that converts fibrinogen to fibrin. This process also requires calcium, which acts as a kind of glue to hold the fibrin monomers to each other to form the polymeric fiber. The fibrin fibers form a loose meshwork that is stabilized by clotting factor XIII. The stabilized meshwork of fibrin fibers traps erythrocytes, thus forming a clot that stops the flow of blood.
Blood clotting is the transformation of liquid blood into a semisolid gel. Clots are made from fibers (polymers) of a protein called fibrin. Fibrin monomers come from an inactive precursor called fibrinogen. The body of the fibrinogen molecule has caps on its ends that mask fibrin-to-fibrin binding sites. If the caps are removed then fibrin monomers polymerize to form fibrin polymers. This process requires thrombin, the enzyme that converts fibrinogen to fibrin. This process also requires calcium, which acts as a kind of glue to hold the fibrin monomers to each other to form the polymeric fiber. The fibrin fibers form a loose meshwork that is stabilized by clotting factor XIII. The stabilized meshwork of fibrin fibers traps erythrocytes, thus forming a clot that stops the flow of blood.

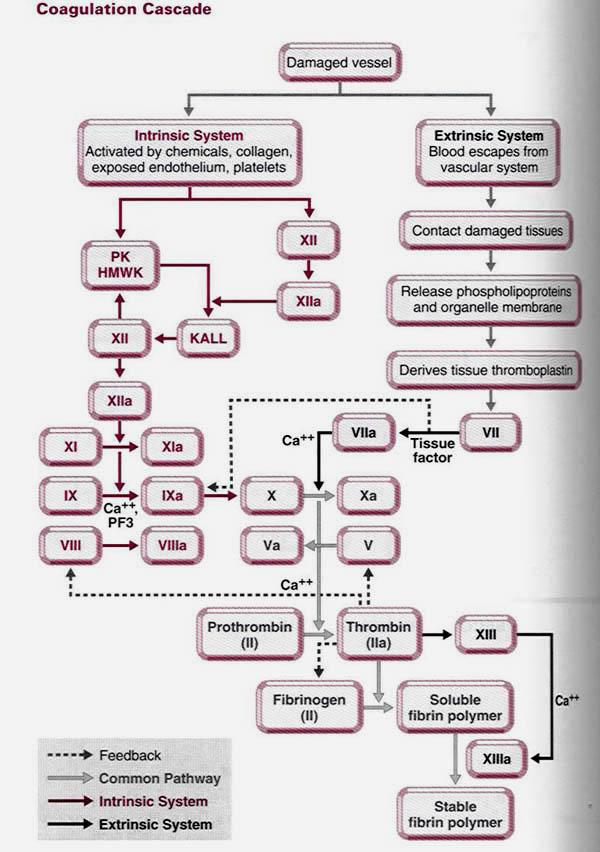
The clotting cascade occurs through two separate pathways that interact, the intrinsic and the extrinsic pathway.
Extrinsic Pathway
The extrinsic pathway is activated by external trauma that causes blood to escape from the vascular system. This pathway is quicker than the intrinsic pathway. It involves factor VII.
Intrinsic Pathway
The intrinsic pathway is activated by trauma inside the vascular system, and is activated by platelets, exposed endothelium, chemicals, or collagen. This pathway is slower than the extrinsic pathway, but more important. It involves factors XII, XI, IX, VIII. Damage to the vessel wall stimulates the activation of a cascade of clotting factors (for the sake of simplicity we will not consider the individual factors). This cascade results in the activation of factor X. Activated factor X is an enzyme that converts prothrombin to thrombin. Thrombin converts fibrinogen to fibrin monomers, which then polymerize in fibrin fibers. Fibrin fibers form a loose meshwork that is stabilized by crosslinks created by factor XIII. The stabilzed meshwork of fibrin fibers is now a clot that traps red blood cells and platelets and thus stops the flow of blood.
The intrinsic pathway is activated by trauma inside the vascular system, and is activated by platelets, exposed endothelium, chemicals, or collagen. This pathway is slower than the extrinsic pathway, but more important. It involves factors XII, XI, IX, VIII. Damage to the vessel wall stimulates the activation of a cascade of clotting factors (for the sake of simplicity we will not consider the individual factors). This cascade results in the activation of factor X. Activated factor X is an enzyme that converts prothrombin to thrombin. Thrombin converts fibrinogen to fibrin monomers, which then polymerize in fibrin fibers. Fibrin fibers form a loose meshwork that is stabilized by crosslinks created by factor XIII. The stabilzed meshwork of fibrin fibers is now a clot that traps red blood cells and platelets and thus stops the flow of blood.
Common Pathway
Both pathways meet and finish the pathway of clot production in what is known as the common pathway. The common pathway involves factors I, II, V, and X.

Summary of blood clotting mechanism
Inhibition of blood clotting
It would be dangerous if blood clotting were to continue to expand beyond the boundaries of the injury. Excessive clotting is inhibited because:
Clotting factors are rapidly inactivated. There are enzymes in the blood that function to inactivate clotting factors. As clotting factors are taken away from the site of injury by the blood stream, they become inactivated by these enzymes. This ensures that clotting will only occur at the site of injury and not progress steadily down the vessel.
Fibrin fibers inhibit the activity of thrombin. Thrombin acts to convert fibrinogen to fibrin, yet fibrin fibers have an inhibitory effect on the activity of thrombin. As the clot grows this inhibition intensifies. This constitutes a negative feedback loop, where the product of thrombin activity (fibrin) feeds back to shut off thrombin.

Clot Removal
Blood clots are designed to be temporary. After the clot has formed, the process of vessel repair begins. Epithelial cells at the margin on the injury undergo cell division. These new cells eventually fill the gap in the vessel created by the injury. Also, cells called fibroblasts are recruited to the area. Fibroblasts form connective tissue that repairs the basement membrane of the vessel (fibroblasts also form scar tissue that may or may not be removed over time). At this point the vessel is healed and the blood clot is no longer needed.
It would be dangerous if blood clotting were to continue to expand beyond the boundaries of the injury. Excessive clotting is inhibited because:
Clotting factors are rapidly inactivated. There are enzymes in the blood that function to inactivate clotting factors. As clotting factors are taken away from the site of injury by the blood stream, they become inactivated by these enzymes. This ensures that clotting will only occur at the site of injury and not progress steadily down the vessel.
Fibrin fibers inhibit the activity of thrombin. Thrombin acts to convert fibrinogen to fibrin, yet fibrin fibers have an inhibitory effect on the activity of thrombin. As the clot grows this inhibition intensifies. This constitutes a negative feedback loop, where the product of thrombin activity (fibrin) feeds back to shut off thrombin.

Blood clots are designed to be temporary. After the clot has formed, the process of vessel repair begins. Epithelial cells at the margin on the injury undergo cell division. These new cells eventually fill the gap in the vessel created by the injury. Also, cells called fibroblasts are recruited to the area. Fibroblasts form connective tissue that repairs the basement membrane of the vessel (fibroblasts also form scar tissue that may or may not be removed over time). At this point the vessel is healed and the blood clot is no longer needed.
The clot itself stimulates the secretion of tissue plasminogen activator (TPA) from the surrounding vascular epithelium. TPA is an enzyme that catalyzes the conversion ofplasminogen to plasmin. Plasminogen is an inactive precursor molecule found in the blood, but plasmin is an enzyme that dissolves clots. Plasmin levels are not very high so clot removal is a slow process. By the time the clot has been completely dissolved by plasmin, the vessel has had a chance to heal itself. In summary, the clot, which forms rapidly, calls for its own destruction by initiating the activation of plasmin.

Anticoagulants are substances that inhibit the process of clotting.
- Heparin
- produced primarily in the liver and lung (usually obtained from pigs or cows)
- acts as an anticoagulant by inhibiting the activity of thrombin
- Used clinically for acute problems, also used to prevent clotting in IVs (heplock)
- fast acting, but short-lived drug. It must be injected to be effective.
- Coumadin (dicoumarol, warfarin)
- taken orally in small doses for long-term control of blood clotting
- acts as an anticoagulant by inhibiting the processing of vitamin K, which is required for the synthesis of several clotting factors including prothrombin.
- It is slow acting, requiring days to have an effect.
- Citrates
- Calcium is required for polymerization of fibrin.
- Citrates bind up (chelate) calcium and thus inhibit the formation of clots
- Citrates are used in long term blood storage.
- Transfusion of large amounts of citrate-containing blood can be dangerous. The citrates chelate calcium in the body and thus disrupt processes such as nerve transmission and muscle contraction.
Blood Clotting Disorders
| Von willebrand disease Animal with this inherited disorder bleed excessively due to an inability to rapidly form blood clots. This defect could be caused by a deficiency of any of the clotting factors. Vitamin K deficiency
Vitamin K is essential to the maturation of several clotting factors including factor X and prothrombin. In the absence of vitamin K these clotting factors are defective and thus inhibit the clotting mechanism.
|
References: Mechanism of blood clotting;http://departments.weber.edu/chpweb/hemophilia/mechanisms_of_blood_coagulation.htm, Homeostasis; http://www.biosbcc.net/doohan/sample/htm/Hemostasis.htm



















