While still struggling to understand on fluid therapy, my attention were hooked on hyperkalemia.
************************************************************
Hyperkalemia is an excessive level of potassium in the bloodstream. Potassium has several important functions in the body. It is essential for the normal functioning of the muscles, heart, and nerves. Potassium helps the body regulate activity of muscle, including the smooth muscle (involuntary muscles, such as the muscles found in the digestive tract), skeletal muscle (voluntary muscles, such as muscles of the extremities and torso), and the muscle of the heart. It is also important for maintaining normal heart electrical rhythm and for normal electrical signals in the nervous system.
Extreme hyperkalemia is a medical emergency due to the risk of potentially fatal abnormal heart rhythms (arrhythmia).
- The normal potassium level in the blood is 3.5-5.0 milliEquivalents per liter (mEq/L).
- Potassium levels between 5.1 mEq/L to 6.0 mEq/L are considered to be mild hyperkalemia.
- Potassium levels of 6.1 mEq/L to 7.0 mEq/L are moderate hyperkalemia, and levels above 7 mEq/L reflect severe hyperkalemia
Normal Potassium Physiology
Potassium is critical for the normal functioning of the muscles, heart, and nerves. It plays an important role in controlling activity of smooth muscle (such as the muscle found in the digestive tract) and skeletal muscle (muscles of the extremities and torso), as well as the muscles of the heart. It is also important for normal transmission of electrical signals throughout the nervous system within the body.
Normal blood levels of potassium are critical for maintaining normal heart electrical rhythm. Both low blood potassium levels (hypokalemia) and high blood potassium levels (hyperkalemia) can lead to abnormal heart rhythms.
The most important clinical effect of hyperkalemia is related to electrical rhythm of the heart. While mild hyperkalemia probably has a limited effect on the heart, moderate hyperkalemia can produce EKG changes (EKG is an electrical reading of the heart muscles), and severe hyperkalemia can cause suppression of electrical activity of the heart and can cause the heart to stop beating.
Another important effect of hyperkalemia is interference with functioning of the skeletal muscles. Hyperkalemic periodic paralysis is a rare inherited disorder in which patients can develop sudden onset of hyperkalemia which in turn causes muscle paralysis. The reason for the muscle paralysis is not clearly understood, but it is probably due to hyperkalemia suppressing the electrical activity of the muscle.
Normal rhythm of the heart
Hyperkalemia rhythm of heart
Causes of hyperkalemia
The major causes of hyperkalemia are kidney dysfunction, diseases of the adrenal gland, potassium sifting out of cells into the blood circulation, and medications.
The majority of potassium within the body (about 98%) is located within cells, with only 2% located in the bloodstream. A number of conditions can cause potassium to move out of the cells into the blood circulation, thereby increasing the measured level of potassium in the blood, even though the total amount of potassium in the body has not changed.
Similarly, any condition in which there is massive tissue destruction can result in elevated levels of blood potassium as the damaged cells release their potassium. Examples of tissue destruction include:
- Trauma
- burns,
- Surgical procedures,
- Destruction of tumor cells or red blood cells
- Rhabdomyolysis (a condition involving destruction of muscle cells that is sometimes associated with muscle injury, alcoholism, or drug abuse).
Moreover, difficulty in drawing blood from veins for testing can traumatize red blood cells, releasing potassium into the serum of the blood sample to cause a falsely elevated reading of hyperkalemia on the blood test.
Any condition that decreases kidney function can result in hyperkalemia, since the kidneys rid the body of excess potassium by excreting it in the urine. Examples of conditions that decrease kidney function are
- glomerulonephritis,
- acute or chronic renal failure,
- transplant rejection
- obstructions within the urinary tract (such as the presence of stones)
The adrenal glands secrete many hormones important for proper body function. Among these is aldosterone, which regulates the retention of sodium and fluid in the kidneys along with the excretion of potassium in the urine. Diseases of the adrenal gland (such as Addison's disease, that causes a decreased aldosterone secretion) lead to a decrease in kidney excretion of potassium resulting in hyperkalemia.
Examples of medications that may lead to elevated potassium levels include:
- Nonsteroidal antiinflammatory drugs (NSAID)
- ACE inhibitors,
- Angiotensin II receptor blockers (ARBs),
- Diuretics.
Hyperkalemia Symptoms
- Irregular heartbeat
- Nausea
- Slow, weak pulse
Diagnosis
ECG test
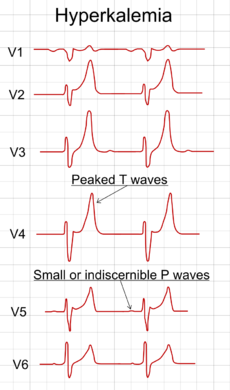
With mild to moderate hyperkalemia, there is reduction of the size of the P wave and development of peaked T waves. Severe hyperkalemia results in a widening of the QRS complex, and the EKG complex can evolve to a sinusoidal shape. There appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization.
Also, (as noted above), hyperkalemia causes an overall membrane depolarization that inactivates many sodium channels. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS complex.

Abnormal rhythm of the heart
Treatment of hyperkalemia
When arrhythmias occur, or when potassium levels exceed 6.5 mmol/l, emergency lowering of potassium levels is mandated. Several agents are used to transiently lower K+ levels. Choice depends on the degree and cause of the hyperkalemia, and other aspects of the patient's condition.
Treatment for acute hyperkalemia
1) Calcium chloride or calcium gluconate
Calcium (Calcium chloride or calcium gluconate) increases threshold potential through a mechanism that is still unclear, thus restoring normal gradient between threshold potential and resting membrane potential, which is elevated abnormally in hyperkalemia. One ampule of Calcium chloride has approximately 3 times more calcium than calcium gluconate. Onset of action is <5 min and lasts about 30-60 min. Doses should be titrated with constant monitoring of ECG changes during administration and the dose should be repeated if ECG changes do not normalize within 3 to 5 min.
2) Insulin
Insulin (e.g. intravenous injection of 10-15 units of regular insulin along with 50ml of 50% dextrose to prevent hypoglycemia) will lead to a shift of potassium ions into cells, secondary to increased activity of the sodium-potassium ATPase. Its effects last a few hours, so it sometimes needs to be repeated while other measures are taken to suppress potassium levels more permanently.
3) Albuterol
Albuterol, Ventolin) is a β2-selective catecholamine that is administered by nebulizer (e.g. 10–20 mg). This drug also lowers blood levels of K+ by promoting its movement into cells.
4) Furosemide (diuretics)
Increase elimination of potassium to the urine
5) Polystyrene sulfonate with sorbitol (Kayexalate) either orally or rectally is widely used with the goal to lower potassium over several hours. Removal of potassium is assumed to require defecation. However, careful clinical trials to demonstrate the effectiveness of Kayexalate are lacking, and there are small risks of necrosis of the colon.
Long term prevention
Preventing recurrence of hyperkalemia typically involves reduction of dietary potassium,removal of an offending medication, and/or the addition of oral bicarbonate or a diuretic (such as furosemide or hydrochlorothiazide). Polystyrene sulfonate and sorbital (Kayexalate) is occasionally used on an ongoing basis to maintain lower serum levels of potassium.
Sources: Wikipedia.net, Hyperkalemia, AAPF, Hyperkalemia, Medline Plus, hyperkalemia, emedicine.net,




























